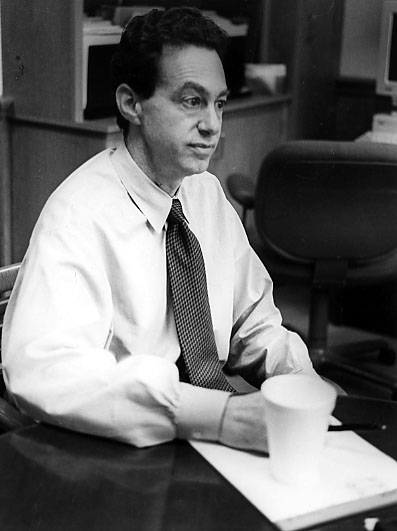
Geoffrey Cole
President, Emerson Hospital
Interviewed March 13, 2001
Concord Oral History Program
Renee Garrelick, Interviewer.
Click here for audio in .mp3 format
 The challenges of administering a community hospital are very daunting at this point at the beginning of a new century, and we should probably not take its existence for granted. It is a difficult time for hospitals. Emerson along with many hospitals in Massachusetts and around the country, but particularly here in Massachusetts have been under tremendous financial stress. Big Medicare cuts in 1998 are continuing on through 2001, and very low payments from the HMOs have combined to put us in a situation where our costs are not being fully covered by the insurers. Providing care, nursing care, drugs, supplies, insurance, and everything you can think of make up the costs of providing care to our communities. We serve 20 towns including Concord. We're slowly digging our way out. We're in the black so far this year in February. We just got the numbers for February. So we're doing better but it's still been very tough on us. We're very much month to month at this point in terms of whether we're in the black or the red.
The challenges of administering a community hospital are very daunting at this point at the beginning of a new century, and we should probably not take its existence for granted. It is a difficult time for hospitals. Emerson along with many hospitals in Massachusetts and around the country, but particularly here in Massachusetts have been under tremendous financial stress. Big Medicare cuts in 1998 are continuing on through 2001, and very low payments from the HMOs have combined to put us in a situation where our costs are not being fully covered by the insurers. Providing care, nursing care, drugs, supplies, insurance, and everything you can think of make up the costs of providing care to our communities. We serve 20 towns including Concord. We're slowly digging our way out. We're in the black so far this year in February. We just got the numbers for February. So we're doing better but it's still been very tough on us. We're very much month to month at this point in terms of whether we're in the black or the red.
In the last year and I think I can say now successfully, we took a group of physicians, Emerson Practice Associates, who were costing the hospital a lot of money and requiring a lot of subsidy from the hospital, and closed that practice. It was 33 physicians, mostly internists and pediatricians but some other specialties as well, in towns all around here not just in Concord, and helped those groups go independent. We lost three doctors out of 33 who said they had to have salary and didn't want to go into private practice. So that's good news. We managed to transition those practices successfully to stay in the various towns, and they're going to keep on using Emerson and they're going to be self-reliant.
Emerson Practice Associates started about ten or eleven years ago before I came. It grew before I came and while I have been here. Well, it grew out of fear as much as anything else. Every hospital was worried that other ones were going to buy up their primary care physicians and there is a great premium on primary care. With more and more HMO medicine, the feeling was the key to being successful for example was to have as many primary care physicians as possible and that they would drive the system and be the cornerstone of it. There has been a growing trend in the exact opposite direction for the last four or five years with people wanting to go directly to specialists relying less on primary care. The health insurers have become more liberal about allowing subscribers to go directly to specialists. So the unique value of primary care diminished somewhat. Also the practices throughout the country have been almost uniformly very hard to make profitable. Let me put it differently, to not lose money. We never sought to make a profit. We wanted merely to cover the costs of employing these folks or at least even to have a loss that is small which we could have sustained for a long period of time, but the losses were large. So we and many hospitals came out the other end saying you know we can't impoverish the core operation of the hospital to what it amounts to subsidies to physician groups. If the practice can't earn enough money to pay a certain salary to a doctor, then the doctor's salary is going to have to go down. And the doctor cannot be looking to the hospital to guarantee his salary. There are productivities dictating a salary of $80,000 but they want us to pay them $130,000 and we can't be making up that difference year after year.
We also found that physicians are no exception certainly to the notion that if you own something you care more about it and you work just a little bit harder than if you're clocking 9 to 5. We needed to change the culture and we tried to change it with small little tweaking of our compensation system but we found that didn't work. So we finally said we'll help you get started but you've got to go into private practice. We'll give you a soft landing and we'll try to make it as easy a transition as we can. It was quite expensive for the hospital to fund that transition, but it was well worth it. It meant that doctors stayed in town. They didn't just give up all hope and start working at levels that were available for peanuts or something which could have been disastrous for Emerson if we had a wholesale exodus of physicians out of our towns. So that's the situation there and those doctors are busy.
We have a couple of good things going on right now. Concord Hillside, a long standing group in town, has just left Lahey and gone independent again which means Emerson will be getting back some of the business that had been slowly trickling out to Lahey. They had been using Emerson for most of their services and each year were taking a little bit more stuff away, and that should all be coming back. There are four new doctors coming both to Bedford and Concord which will be very good in strengthening the primary care physician base here in town.
I just met with our whole medical staff at noon today and commended the article in today's Boston Globe because I thought it was a fascinating article. I was also happy to tell them we were not one of those hospitals losing patients to the city teaching hospitals, but in fact we've seen small gains over the last couple of years. The most interesting fact in there is that in Massachusetts about 40% of hospital admissions go to teaching hospitals versus 18% nationally. So people use teaching hospitals much more in Massachusetts than anywhere else in the country, and I wasn't surprised because there is such a concentration of them in eastern Massachusetts. It does increase the cost of care because teaching hospitals are always going to be more expensive than other hospitals because they have the additional mission of teaching a whole new cadre of physicians, and that gets expensive.
Emerson always struggles with that. There are always going to be people in our area who go downtown, but we've held our own better than most and our relationship with the Mass General and the Brigham is a loose one. We're not owned by them in any way but we're affiliated with them. That has resulted in the cancer center that we partner with at Mass General and in the next several years we will try a partnership with Dana Farber. The program for high-risk mothers that we're doing with the Brigham and the pediatric subspecialty clinics that we're doing with Mass General are at Emerson, so we have a whole range of things that bring world class care to our community so people don't feel they have to go downtown. They can get the kind of care they would get downtown out here at Emerson. Moving away from the heritage that Emerson has which is a perfectly lovely one, but is not a very helpful one in this day and age which is as a quaint "cottage house" as they used to call it. They were really way stations. We've done lots of surveys and focus groups with people in towns around here, and people really want the high touch, the personal touch of a nurse, which is very high, but they don't want to give up anything to get that, they don't want to forego the best technology, the best physicians, etc. so we have to be high tech. We have to keep pace with the downtown hospitals. We don't do everything the downtown hospitals do, but 90% of things where we overlap with the downtown hospitals we do it identical. We use the same technology, the same nurses with the same skills, doctors with the same training, then people expect more personal care because they are at a community hospital not downtown. The community hospital is expected to have more personality.
The Bethke Cancer Center that opened about three or four years ago is a relief to people to not have to go downtown for treatment. It is very hard if you have to get chemotherapy or radiation therapy several times a week in many cases and it's a nightmare. Lots of people have to go downtown. We're able to do that jointly with Mass General and give people a high level of comfort and satisfaction. It is a very cutting edge program. We see between 30 or 40 patients a day for radiation. And more importantly we're able to give comprehensive care now to patients. There is no modality of cancer care for 90%+ of cancer patients, and we can't manage completely at Emerson but we provide really state-of-the-art, modern and comprehensive cancer care here. There are certain things we don't do. We don't do pediatric cancers here. But most everything we handle at a very high level. So that's the model we're increasingly using.
With the Dana Farber affiliation we will now be providing all the same research clinical protocols and investigational treatments that are available at Dana Farber which means we will really be on the cutting edge nationally right at Emerson. So that's just tremendous. We want to continue replicating that model in different clinical areas over time.
The other thing we're doing a lot of is trying to expand geographically into the towns that are growing around here. We opened a center in Westford that's very extensive. We're just now opening a center in Groton with physicians, lab, and radiology. One thing Emerson needs to do is grow. We have a lot of fixed costs as do most institutions, but we need to be just as busy as we can possibly be. We have been busy, but we need to stay busy and keep growing and get the payments back to where they need to be, that's really the solution to financial peacefulness. Being bigger means being more relevant to our community which is what we're here to be. To have fewer people feel they have to be leave Concord for their care, we're really meeting our mission fundamentally. So there is kind of a happy coincidence of what we need to do to stay financially stable and we need to do for the public health, then it's the right thing to do for the public health of the towns we serve. Those towns include Acton, Carlisle, Lincoln, Sudbury, Concord, Bedford, Lexington, Boxborough, Harvard, Groton, Westford, Littleton.
Some of the small community hospitals have had to close over the last ten years particularly in the last year or two. None around here had to close. We do have a large group of physicians at Nashoba Hospital in Ayer who are going to be moving most of their business to Emerson starting shortly. They will be moving to our center in Groton. It was not our purpose to imperil Nashoba Hospital. It may be one effect. This group came to us actually because they were concerned that Nashoba wasn't growing the way they were and had been hearing good things about Emerson. When we built our center I think that was the last straw for them, and they decided to come see if we were interested in having the physicians at our hospital and we said, of course. They're going to continue to use Nashoba, but they're aiming to send at least half of their business or more over here. That will strengthen Emerson. That will strengthen us in those towns which are growing very fast. And it will bring more business to the hospital and keep us strong to keep our mission for everybody.
Development and fundraising has not been a huge part of the formula for us until recently. I think what you're seeing now is more and more hospitals really raising the level of fundraising. We're doing a capital campaign right now to raise $8.7 million for the hospital, and we're over $6 million there in pledges as of this week. So we're doing great. We haven't even begun the public phase of the campaign. Right now we've talking mostly to board members and corporators and physicians, people closer in to the hospital, but we're going to a fully public phase later this summer. I think it's going to be extremely important in the future for hospitals. Philanthropy is going to be a main source. It may have to be relied on to make up that difference and it'll mean much more intense effort at it. You could be almost in what amounts to a perpetual campaign. Then we have routine fundraising. We raise about $1 million a year depending on how you count the money. Some of it comes in bequests and you don't get it until somebody dies, then it gets complicated. But that's been going on for many years. We've seen a good couple of percents increase every year in that amount. I'd like to get that amount to $2 or $3 million every year, not as a special capital campaign but just routine annual gifts to the hospital. But to do that will take a much bigger effort. But you're hearing that more and more with hospitals all over the country. We have a budget of about $110 million a year, and our philanthropy provides a small part of that. It is much appreciated and it makes a big difference but it's not been a huge amount of the pie.
I don't sense too much that doctors in Massachusetts feel their incomes have not risen proportionately to costs. I don't sense much of that sort of we and they. But, there is a big problem with physician compensation in Massachusetts. We're starting to see a lot of doctors leave the state. Harvard Medical School has seen more and more doctors leave. The doctor might say I'd love to be on the faculty at Harvard, but I just got an offer from the University of Texas and I got three kids to put through school and I can buy a house with six bedrooms for less, etc., and we hear that from people downtown. We experience that to some extent being in a very expensive set of towns around there. It has been a very hard thing for doctors. With only a few exceptions like surgery and a couple of other subspecialties, doctors' income have really dropped like a rock over the last 10 or 15 years. At the same time you're seeing all the high tech entrepreneurs getting rich. You see some doctors now in middle age and older who I think they sort of got a raw deal. They signed up for one thing and it turned out to be something different. Younger physicians tend to be much clearer about why they're getting into the profession and aren't as angry as a group. It's more of a sense that I could have done something else but I really wanted to work with people, I wanted to be a doctor, I knew I'd make a good income but I'd never be like the guy who owns the dot.com company or whatever. There are big differences generationally. Then you have doctors who are 60 or over who were around when medicine was still paying well and have done just fine and they're retiring happy. So it's a very mixed kind of complicated group. I think doctors are fighting hard and we have to fight for them because if we have doctors leaving the state, it's going to hurt the hospital. If all the radiologists decided they can't make a living around here, we're going to be in trouble. Or any other specialist for that matter. So the hospital has an interest in making sure the health plans and Medicare and others are paying sufficiently, particularly to live in an area as expensive as this. We can't have doctors living 45 minutes away from here. That means they have to have an income that would allow them to raise a family out here.
Business practices have always applied to medicine. We're not a for-profit hospital. We don't have shareholders and we don't need to make huge profit margins. We just need to make enough to keep this place able to reinvest in technology and stay modern and meet the salary needs of 1350 people who work here. We're a big employer. We're certainly one of the biggest in town. What's interesting is that hospitals are businesses and they're also not businesses. They always will be both. We don't exist to make money. We exist to provide healthcare and we only need to make money to meet that mission. So in that sense we're fundamentally not a business except we have all the elements of a business. We have employees, we have capital needs, we have a budget, we have suppliers and the whole bit. So you have to keep at all times sort of a split mind about both. That's one of the things I find very interesting about the job actually.
The fellow who runs Mass General, Sam Thier, one of the pre-eminent physicians in the United States, talks about hospitals in a more cold-light business way than I'm used to. He's a world famous clinician so you never know where it's going to come from. Sometimes it's the clinical people who are so business like, and sometimes its the business people who worry most about quality of care, and it's fascinating.
My background is in public health. I learned business along the way and got a good training in Berkeley in health care finance but it was fundamentally in epidemiology and public health. It's not clinical medicine, but it's a lot closer to clinical medicine than it is to business.
I'm going to be president of the Mass Hospital Association in a couple of months. That will involve a fair amount of my time for a year. It's a great honor. It's the association that represents all the hospitals in Massachusetts. I've been fairly active the last couple of years. I got nominated a year or two ago to be president-elect when the current president leaves in June. So I'll be public spokesman for hospitals in the state. I've been doing a lot of lobbying and a lot of public speaking which I already do a fair amount of. I've been doing that on behalf of Emerson, but now during this year I will be serving hospitals in general. I'm going down to Washington, and there's a lot on the table right now legislatively regarding hospitals.
The lobbying efforts with the legislators are trying to have them understand what's going on for hospitals and how important they are and that we're not crying wolf, that these are real serious structural problems right now. Many hospitals have gone under recently and when they do it really gets people's attention. Also the hospitals that are remaining in the state have never been busier. So to be as busy as we are and then to be losing money creates a real paradox and one that really points out poignantly to anybody that's really paying attention that there is something fundamentally wrong here. It was one thing 20 or 30 years ago when there was a big over supply of hospitals and beds, they would say oh, you guys are fat, and there are too many of you anyway, so if half or a third of you went under, then those that remain will be fine. Well, here we are. Hospitals are very busy. There are fewer of them that are run efficiently. I'm very confident when I say we're not fat at all. We're very busy and some would say too busy, but still we're barely in the black right now. In any month there is that risk of going back into the red. By being in the black we're actually doing better than most hospitals in Massachusetts. Sixty plus percent of hospitals in Massachusetts are still in the red so far this year.
Some legislators understand the issues and some don't. Part of this job as Emerson CEO and also in my MHA hat is to educate people. Hospitals get a good hearing. I certainly always do with our state reps. We are big employers and we're critical to public services and we are capable of doing it. We're not government entities that can be bailed out. We're private not for profit companies that are critical to the public. Getting the reality or potential urgency of the situation to people, some get it right away and with some it takes a lot of effort. We're fighting real hard right now to inform about the uncompensated care pool where there is a certain way in which hospitals in areas with less uncompensated care or fewer people with charity care get help or subsidized to do charity care. I have no problem with that subsidy. I think it's a kind of socialized care of the uninsured. The problem in most of the states in the country is that the state takes the lion's share of the responsibility, not the hospitals themselves. In Massachusetts hospitals take most of the costs of this uncompensated care pool, and it's been a terrible burdensome debt that's like a tax for us. We're paying almost $4 million a year to this pool, and we probably provide a form of uncompensated care much less than that. And we see everybody that comes to the hospital. Nobody is ever turned away. But for us to be losing money, we still have to pay at the time we're losing money a fairly large amount because the state won't do what 48 other states are already doing. We have a big push going on right now until June to try to get legislation passed to take this huge burden off hospitals like Emerson.
Medical costs in Massachusetts are high and the reason was described in that article today in the Boston Globe is not that hospitals don't run efficiently in Massachusetts. We compare very favorably either community hospital to community hospital or teaching hospital to teaching hospital, but the percentage of people who use teaching hospitals is so much higher in Massachusetts. It's almost three times as high as it is anywhere else in the country. These hospitals will always be higher because they're efficient, but they are just different creatures. They have other things they have to do that raise their costs. That's something that may eventually have to be addressed. There's been talk about putting together a health plan that would give disincentives to people for not going to teaching hospitals for things you don't need a teaching hospital for. Examples given were getting a gall bladder taken out or getting a hip replaced. That might work. The question is what do people want? If people want access to Mass General and Brigham and Beth Israel for every little thing, the marketplace is going to rule. It is ruling right now. People want to go wherever they can.
Some teaching hospitals are moving out to the suburbs. There are actually more and more moving out. We've managed so far to resist being eaten alive by the downtown hospitals, part of it by working with them so we're not fighting them.
There are more and more health institutions in this community particularly with an aging population. We've got continuing care, adult communities where people can get different levels of health care as they get older. There is a tremendous move in this industry and it will keep on growing. They are expensive typically. Even the least expensive of them are pretty expensive. It's a pretty natural thing for a town like Concord or Lincoln or Carlisle. You have Sunrise, New England Deaconess with Newbury Court, Volunteers of America, Walden Healthcare. We work with them a lot. We're always having to coordinate with them and patients frequently come to Emerson from one of these institutions and then go back. Every day we're having to find placements for people in nursing homes. The hospital has its own skilled nursing level on the sixth floor of the Wheeler Building. It is called a transitional care unit which is for patients who don't need acute care any more, but they are well enough they can be in a lower level care and need a week or two weeks of rehab. It is the bridge either back to home or to a longer term care or to a senior housing center. We have social workers here working on case management helping to figure out what the plan should be for that patient in the future. We also have a home health care service and they make about 60,000-70,000 visits a year. We have 80 home health nurses and aides in their cars all day long seeing people in their homes.
We have a busy hospice program and that is really part of home care because most of the hospice is done in the home. There are hospice programs that are hospital based where people actually can come and be in a hospice overnight for a period of time. Those are a little less common. We don't do that presently. Of course, with the growing cancer service, cancer and hospice are closely linked. It's been a wonderful service and a tremendous way to meet the needs of patients in our community.