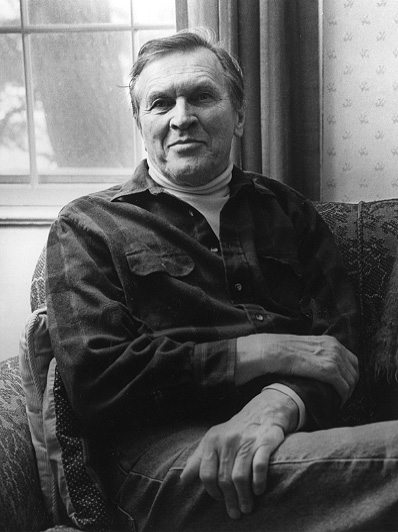
Dr. Donnell Boardman, Internist
Acton Common
Age 75
Interviewed November 9, 1988
Concord Oral History Program
Renee Garrelick, Interviewer.
Perspective on Primary Care Medicine.
Click here for audio in .mp3 format.
 -- Efforts to begin prepaid group practice
-- Efforts to begin prepaid group practice -- House calls
-- Impact of technology on patient-doctor relationship; medical malpractice
-- Formation of the Acton Medical Associates
-- Introduction of Boston University School of Medicine preceptorship at Emerson Hospital
-- Emerson Hospital staff
-- Pacifism, medical service during World War II in Japanese Relocation Camps. Atomic bomb explosion
-- Quaker Mission Hospital in Kenya
-- Physicians for Social Responsibility
-- Study of human effects of ionizing radiation
-- Teenage drug problem, late 1960s
At the end of World War II, my wife and I had thought to move
into the Boston area rather than the New York area where we had
both grown up because academically it was more favorable and
because you could live in the country and still be close enough to
the metropolitan center and the academic center. We came with
four small children. I came first with two run-about children,
and we slept our first night here in the old homestead across from
the library. When there was no fire in October, we slept on the
floor in the dining room of a house that I bought before the
family ever saw it. The two children and I had breakfast at
Howard Johnson's, a new restaurant in Concord. It had just
started up at that time. Mother and months-old twins arrived
later the next day.
We came to Acton because it was in the country but within
striking distance of Boston's medical, academic, and cultural
centers. There were only 3200 people in Acton at that time. It
was a nice country village with apple orchards, dairy farmers, and
truck farmers. A few people worked in Boston, but not very many.
It was our intent to become a small group practicing medicine
hopefully with a patient-consumer cooperative prepaid medical
plan. As time developed it turned out that it was a group of two
offices, one in Maynard and one in Littleton, and two hospitals --
Emerson Hospital in Concord and the other what was known as the
Mass. Memorial Hospital in Boston, part of Boston University. I
was running between two offices and two hospitals. About four
years later Dr. Henry Stimpson Harvey joined me because he was
also looking for a country practice near a metropolitan center,
and we had other similar interests.
The United Cooperative Society was a consumer cooperative of
groceries, hardware, coal, and oil started by the Finns who lived
in Maynard while they worked at the American Woolen Company. That
cooperative started really because the mill workers found that
most of their paycheck provided by the American Woolen Company
went back to the American Woolen Company because they had to get
all things at the company store and other places that took
advantage of their sort-of isolation. They got together to
develop the cooperative endeavor so that they could control the
prices that they had to pay for food and the common household
needs. Indeed, they found it made an enormous difference, and the
Cooperative Society was extremely successful for at least 10 or 20
years after we came in the 1940's. It really died when most of
the younger generation of Finns who had any get-up-and-go got up
and left. That left the older people, the diminishing number of
Finns and the diminishing number of mill workers as a central
core. A lot of people who moved into the area, which included all
the towns around Maynard, had an intellectual and ideological
interest in cooperatives, but they didn't have the tight-knit
cohesiveness provided by the American Woolen Company and by the
Finns. So it gradually became less and less loyally supported.
At the same time the Stop & Shop, the supermarkets, began to move
in, and I think the first one was the A & P and its prices in
Maynard were substantially lower than they were in Concord because
they were trying to out-compete the cooperative. Well, with one
thing or another, competition did prove to be too much for the
Cooperative Society, and it succumbed. One of the reasons we came
was not only the Cooperative Society but at that time we were
looking into seriously and hard at getting pre-paid medical care,
but their whole idea of medical economics was very different than
even mine as an emerging idealistic dreamer. With four small
children, even in 1946, I thought that $8000 a year was pretty
meager for a well-trained physician; but the salary of the general
manager of the cooperative, which I think by that time was a
million dollar a year proposition, was only $5000. They couldn't
see paying a young man anything like that figure, so we never came
to any kind of an agreement, and the prepayment never materialized
until some 30 years later.
There were about five doctors in Maynard when I arrived and
most of them with one exception were significantly older than I.
Only one of them had any access to Emerson Hospital, and he did
not make use of it, so that the medical care provided in Maynard
particularly was, should we say, limited. For serious illnesses
patients found that they went even beyond Emerson Hospital. They
went into Boston because the local physicians, if they referred
them to Emerson Hospital, were likely to lose their patients to
Emerson Hospital based physicians. Even at that time though
Concord and other towns used Boston at least as much as they used
Emerson Hospital. Emerson Hospital itself had an ambiguous
reputation with the population. There were some who felt that the
patients went there only to die or to prepare to die. I don't
think that was fair, but it was understandable because since it
was limited, people usually got there too late. It seemed to me
it was very obvious that Emerson Hospital had tremendous
potential. Charlie Duston was a very competent technician and a
very competent businessman, and really did a lot to improve the
image of Emerson Hospital.
When I first started, my office was on Nason Street in
Maynard over the A & P. We came to the area, as I said, because
of the possibility of cooperative prepaid medicine. My interest
had led me up to the Boston area because I had some medical school
training in Boston under Paul Dudley White, the cardiologist, and
a number of others; but I had also known several other MGH doctors
who had been interested in the White Cross, which was the first
prepaid group practice started just before World War II. Dr.
Edward Young thought that the White Cross itself was a war
casualty, that all the doctors who were participating were
eligible for the service; and they got pulled out, and there was
no one to provide the service. Therefore, it fell apart. Interestingly enough, he, Alan Butler, Hugh Cabot and several others
were called up before the medical society in the early 1940's and
were asked why they shouldn't be thrown out of the medical society
because they were practicing a socialized, almost communist
concept of medical practice. They weathered that, but the drain
on the doctor participants yielded to World War II. They were
quite interested in my coming into the area with this interest,
and so they were very nice. Robert DeNormandie was an obstetrician who lived in Lincoln and was probably the dean of clinical
obstetrics in the greater Boston area at that time. He did a lot
to help introduce me and my credentials to a blue-stocking
population in Concord and Lincoln, so that I garnered a number of
families of the cultured, educated, and sophisticated population
of those towns. At the same time, it was well known among Finnish
mill workers that I was coming equally well-approved, so that I
got started fairly promptly. My wife and I celebrated when I had
a day that grossed $30 -- that was a big event!
Night calls, it always seemed to me, were extremely
profitable to physicians. I sort of deplore the loss of house
calls in the present day because it seems that doctors really
never get to know their patients if they never go into their
homes. In a period of high tech and computerized billing, this
separates the doctor from the real essence of medical practice.
What we were saying about how sick we are between the ears is ever
so manifest. I remember getting called to see a man who had a
fever just outside the center of town. He was desperately sick,
103.6 degree temperature and his whole body flaming red and
beginning to pustulate. He was a man in his late twenties with
chicken pox. He survived, but I learned not only about that but
about his children and about his wife, who turned out to be at
that time in and out of a sort-of schizophrenic behavior. I
learned about how that family lived. It was extraordinary. You
go and see people in their homes and they are very different than
they are in the office. Night calls were particularly revealing
in that way.
I think that medicine has lost a lot because doctors have
gotten caught up so much, necessarily perhaps, with high
technology which has been developed by the electronics industries,
but to the detriment of their relationship with people and the
people's family constellation -- all of which contributes to the
illness. Yes, I think house calls and night calls were
fascinating. It got a little irksome when you got called by the
police to make a house call and then as happened to be on one
occasion in response to the police having called me, I was
hurrying to the house and had one of the town police cars stop me
for speeding. That was really annoying, but usually it was a very
interesting thing.
There is a very famous caricature cartoon that shows the
patient lying in bed with his head swathed in bandages, the doctor
standing by the bedside, his doctor's bag opened, the stethoscope
drooping out, and the doctor holding a pen and wetting it to his
lips as he writes on the white wall behind the patient his bill
for his services. He has got a whole lot of things itemized. The
point being that the doctor makes his living at the cost of the
patient's discomfort. On the other hand, there is no question
that an eye-to-eye and face-to-face confrontation of patient and
doctor has a disciplinary effect on the doctor's charges and his
compassion. If he really finds that what he is asking for hurts
the patient because he sees it on his face, then he is able to
modify it. The introduction of third-party payments has removed
all that. Most people, including the doctors, don't have any idea
what the costs are that are being generated in a doctor-patient
relationship in the HMO-type of practice.
On the other hand, the fact that big business has moved in
and complicated medical care, there is an enormous overhead you
have to pay for the business administrators. The high-tech, as I
have indicated before, has gotten to be so expensive. If you have
an expensive diagnostic test machine in your office, you have to
use that machine to pay for that machine, and you have to charge
the patient for it. You use it -- sometimes it helps and
sometimes it confirms. Usually it does no more than to confirm
the doctor's decision on whether the patient does or indeed does
not have what the test is supposed to show. It all separates the
doctor from the patient. To my mind, that is the essence of
medical care and indeed in human relations -- one-to-one sharing
of the responsibility of the patient's malady. If the doctor
doesn't encourage the patient to meet his misfortune and meet his
disease with him, then he is going to have less success and
perhaps be another failure. It seems to me if you would list the
patient's help in his cure, then you have pretty well insured that
patient as a colleague and as a friend and not an adversary that
you are going to meet in court over a medical legal practice.
I have always felt that generally speaking a patient that
develops medical malpractice has got a basis. It usually is a misadventure in the medical management, irrespective of the fact
that the patient also may or may not have had a fatal or a
crippling disease; but usually there is a mistake of one sort of
another. The reason it gets to court is because there has also
been an alienation between doctor and patient. This is particularly true in a complex system whereby the disease is treated by a
team of doctors, none of whom address themselves to the care of
the patient. They are only treating the disease, and the patient
and the family very often feel left out and then they begin to
have doubts. Then they begin to ask questions, and there is
always somebody to go to and they'll say, "Yes, you have gotten a
rough deal." That is what seems to me a major disaster. This is
after all the common phenomenon in our socio-economic society
anyhow. There is very little trust now. You have to have a
credit card. The idea of going in and saying, "I am me, I've been
around and you've been around for 20 years, we know each other, we
trust each other," is a thing of the past. There is just no more
of a warm vibrant community, unity, and confidence, and it is very
sad because it lends to the climate of distrust in every aspect of
our human relations.
As you know the Acton Medical Associates now has 14 or 15
doctors. While I was there we never got bigger than six or seven.
Acton Medical Associates began in 1957 but it was really formed
when Ed Bell joined us in 1954. Henry Harvey came in 1952. Two
was a partnership and three qualified for a group or an
association. We paid $3,000 for the land, it was too much for
that piece of property, but I think it is fair to say that it is
probably valued at 50 to 100 times what we paid for it now. The
building has been expanded, I should say doubled and then
quadrupled in size, so I guess it was a pretty frugal and
worthwhile business venture.
We felt that group practice was very important. There
should be a free interplay between covering for one another. As
the group developed the group was interested, even as I had been
interested, in having a personal one-to-one relationship, so we
always asked patients to choose one of the doctors to be their
personal physician, or for the family there would be a family physician. If they, over a period of time, wanted to change that,
they should feel perfectly free to do so, but there should be a
one-to-one relationship. That survived pretty well even when
there were five and six members of the group. We all had our own
loyal following, all of whom were perfectly willing to accept one
of the others as a replacement for on-call, vacations, holidays,
or things of that sort. There was always a one-to-one relationship, and that as I said survived as long as I was there.
I joined the staff at Boston University and in 1948 and did
some outpatient teaching three times a week throughout the school
year. Then some six or seven years later, since I was a great
advocate of country practice and the practicing physician in a
semi-rural area having at least a toe-hold in an academic
situation, I wanted to promulgate that. So I went and talked to
Dean Jim Faulker at B.U. School of Medicine, and he was very
helpful encouraging me to start what was called a "preceptorship,"
which got fourth-year medical students to use one of their elected
periods to come out and work with me as preceptor to learn about
the clinical practice of medicine in a community that included
industrial medicine, school physician, sports medicine, as well as
clinical practice in office, house calls, and hospital. The first
year I tried to introduce this at the Emerson Hospital there was
one member of the staff who was outraged at the damn thing and
then talked to all the doctors about the ill-advisability of doing
this and suggested that I was just using medical students to spy
out my colleagues so I could get the advantage of them. When it
came to a vote, the vote turned out to be, I think, thirteen to
one. Within weeks the doctors in Boston and in the teaching
hospitals all around who had any contact with the Emerson Hospital
staff members were asking questions -- "What happened to Emerson
Hospital? Why did you lose such a wonderful opportunity?" The
next year it got started, and it went for a good 10 years from
1953-1963 as long as I was at B.U., and we really had a
fascinating time. Students were very enthusiastic. They proved to
be good learners, and they kept not only the members of the Acton
Medical Associates, which was growing at the same time, but also
members of the staff at Emerson Hospital on their toes. Witness to the fact that even though that preceptorship came to an end, it
has since been re-established by younger members of the Emerson
Hospital staff so that I felt it was a good thing well worth
starting. It was lots of fun -- just lots of fun.
I served on the Emerson staff essentially from 1946 to 1986.
I went away for a couple of years in 1978 to 1980 and then came
back and practiced more or less on my own but under the roof of
and with all the office and nursing support of the Acton Medical
Associates, but I did not rejoin the Associates. So I was there
for 40 years.
I had a very clear idea, at least I thought it was a very
clear idea, of what practice could be when I came to Emerson. I
came to Emerson because it was in the country and close enough to
be associated with teaching and academic medicine in the city. I
came, as I look back at it, with a good deal of self-assurance and
confidence in the idea and I made it very clear -- there wasn't
any question in my mind. Older men who had been themselves
well-trained, many of them at Harvard, took some exception to my
being outspoken and my being ambitious in this way. Yes, I was
quite outspoken. The laboratory at Emerson consisted of a
part-time technician who stopped on his way back home from another
hospital laboratory and did the laboratory work for the hospital
between 5:00 and 6:30 in the evening. My immediate reaction was,
"That's not enough!" I said so. Well, I made a number of other
comments which may have touched closer to home. At the end of the
year the chairman of the board of trustees caught me in the car at
the hospital and asked me whether I thought there was any reason
why the board of trustees should reappoint me to the staff. I
just stopped in the car and said, "Can you give me a reason why
they shouldn't?" He didn't answer, and I don't know what he was
looking for when he asked the question. The question or the
appointment never came up again.
It is interesting, you know, I never did raise questions that
were totally unacceptable or unthinkable by my colleagues.
Usually when I raised an issue, there sort of was a startled,
electric silence after I asked the question but people would come
up to me after the meeting broke up and as we walked down the corridor said, "Don, I am so glad you brought that up ..." I
said, "Where were you? I didn't hear you speak up and defend ...
"Well, you know ......" And this happened over and over again,
but it was a good relationship. Once the Acton Medical Associates
got established, just the fact that they were there, my partners
really didn't have to speak up because it was known that they were
my partners, you see. I almost never asked any questions at staff
meetings without having sort of fielded a sense on this subject
with my partners and with one or two other people. The staff
really did get to be a lot more liberal and a lot more open as
years went by. Within the next ten years, not only Acton Medical
Associates but lots of new doctors came who were much more
receptive to new ideas. Witness to the fact that Emerson is now a
very impressive, almost top-flight care at a time when hospitals
are having a rough time.
I have gotten in and out of jail I might say on social
issues. Yes, I spent a night in jail in Washington, D.C. I was
sitting on the sidewalk in front of Mr. Nixon holding him in the
light as the Quakers say. That just so happened to have been the
weekend before Washington D.C. law and order was expecting the big
demonstration in Washington which took place, and so I have always
felt that when they picked up something like 100 Quakers that
Sunday they did so to serve as a warning to those who were going
to come the next week.
If World War II had come much earlier, I wouldn't have been
as well prepared to provide service to my fellow man because I
wouldn't have completed my formal medical training. If it had
come a little bit later, I wouldn't have had the same opportunity
to take a position. Most particularly, the fact that I had had my
post-graduate training in medicine, so that I was fully prepared
to take on a job that the government could use. They could see
that they were going to need doctors, whether it was in the
military or out of the military. So they made good use of the
fact that I was a qualified doctor. When I found out that the
American Friends Service Committee were helping conscientious
objectors, I got in touch with them and they said, "Go and ask the
Civil Service Commission about the Japanese Relocation Camps." They were delighted. Most of the doctors they had were really
marginal at best. I said I am a young man and I recognize the
word in an emergency and I am ready to go anywhere, do anything
and be moved around, and my wife is quite understanding and is
willing to cooperate." We went to be troubleshooters for the War
Relocation Authority, which was designed under the Department of
the Interior, under Harold Ickes who was just a delightful person
to work under. He had a vision -- you could feel it even in the
ranks way down where we were in the mud of Arkansas, in the desert
of Arizona, to provide the necessaries of medical care to the
Japanese Americans and the Japanese who had no citizenship that
were moved out to the West Coast war zones and were put into these
camps.
The physical insult and hurt was far less than the
psychological, the economic, and the social isolation -- focusing
on them just because they were of Japanese heritage. It was
devistating to a self-respecting people who had really made their
mark and contributed enormously to the wealth of California
particularly as farmers. They were just very good industrious
people. Well, in the end it turned out there were ten camps, and
I served in seven or eight of them. There was one time I thought
I knew more Japanese-Americans on first-name basis than most of
the Japanese-Americans in the country and wherever I went it was
to go to a place of greater urgency and greater need than where I
already was, so it was a great experience. I always felt it was
by far the most creative way to spend war years for young men that
could be done. By and large almost every young man who lives in
the country through an era of war is a war victim. They are
scarred for life by the experience they had closely associated
with the war, whether they served in the military or not. The
compromises, the attitudes of mind are so disforming and so
warping from a creative, positive way of life, that it is
devastating. I felt by far that this was the least injurious way.
As I said, I always felt that I was particularly favored.
I went off to the first assignment leaving Elizabeth and the
new baby, a year-old baby behind, and she joined me about three or
four months later. We were discussing this the other day with this chap and his boy visiting us today, we were talking about how
many of the camps she had been to. And it turned out that she
also had been in six. She did one stretch of teaching in the high
school, teaching English to the students, one of whom later was a
medical school student, and having been taught in high school by
my wife was taught in medical school by me. Several others, one
who was president of the class told me that he thought that
evacuation of the Japanese was one of the best opportunities of
his life. It had gotten him away from just the parochial scene in
California and he was headed off to an eastern college.
There were those who felt that this was quite a positive
experience; but there were a lot of people, particularly the older
people, who were much hurt by it, and their self confidence was
really shattered. So it was a disaster. But I'm delighted that
even 40 years later it has been acknowledged ultimately and
ostensibly supposed to be given some kind of compensation.
I was there when the atomic bomb was dropped. We were in
Tule Lake, which is the largest and the last of the camps. There
were 18,000 in Tule Lake, and we were there for something over a
year at the end of the three and a half years. My wife was
pregnant with twins and had two runabout children and we got Mrs.
Sakari a Japanese born woman who knew very little English but just
enough to make do with Elizabeth's help to communicate with one
another.
August 5 came, and a train came down the track toward the
camp down the valley blowing it's whistle until the steam ran out
and the whistle just drooped out and died; and the news came
almost instantaneously from up in the camps that Hiroshima had
been bombed. Elizabeth turned to Mrs. Sakari and said "Mrs.
Sakari, don't you come from Hiroshima?" And she said, "Yes, I do."
Elizabeth said, "You have family?" She said, "Two sons, my
parents and all my brothers and sisters." Elizabeth said "Oh,
dear, perhaps you should go home and be with your husband and
family." She said, "No, I take care of the children." By this
time the twins had been born, so she got all four of the children
taken care of and then she said, "Perhaps I go home." It took
time for everybody to begin to understand the full implications of
this, and it was a sorry time.
Mrs. Sakari was released because the war was over and went
back to Sacramento, and a good friend of hers who stayed in camp
working with another family came and checked in on Mrs. Boardman
and her four babies. She looked around and said, "You can't do
this, you need Mrs. Sakari, I send my daughter." So Mrs. Sakari
came back and much to the surprise of the military police who sent
word, "There's a Jap out here who says she just got out of the
camp and now she wants to come back in, is that all right?" So my
wife went out and said it was all right that she was coming to
help her. So that was our first intimate association and our
first concern with radiation and the nuclear bomb and all that
sort of thing.
To my knowledge her family lived in the center of Hiroshima,
and we never heard a word. Very little was known about the true
dimensions of that thing for five years. Nothing came out of the
military. We never knew their fate. We assumed, of course, that
Mrs. Sakari lost all her family and her two sons, but we never
knew.
We didn't become Quakers until after the Korean War because I
didn't want any question for the Selective Service Board about
joining a peace church to avoid the draft. It was a special
doctors' draft, the Korean War. I got called up and submitted a
conscientious objector plea in which I sent a copy of what I had
written ten years earlier and said nothing has happened in the
intermittent ten years to do more than confirm my opinion. They
wrote back and classified me as too old to fight. After that we
joined the Friends, and through the Friends we learned about the
Quaker Mission Hospital in Kenya. I don't really know why it
seemed like such a good idea to both me and my wife to go. They
had a doctor that was finishing up and two other doctors that were
going three months later, and I said it was obvious they needed
some kind of liaison, so I volunteered, having had a splendid
time. I enjoyed it so much that I kept talking about it, so that
when I got to be 65, my wife thought it would be a good way for me
to get out from under the Acton Medical Associates. Given my
temperament, she thought that it was unlikely that I could truly
retire from the Acton participation staying there, and I agreed,
so we went off for two years.
When we came back from Africa, the Physicians for Social
Responsibility was being reactivated by Helen Caldicott, the
Australian pediatrician at the Children's Hospital, who had been
concerned with the uranium miners in Australia. She and her
husband both came to teaching positions, but she became very much
concerned with nuclear energy, as indeed a lot of people were.
The atomic veterans had just come to recognize themselves after a
25 year silence. They were just beginning to be aware of the fact
that they had been exposed and that many of them who had no
connection with one another, because there was very little buddy
activity generated or encouraged among atomic veterans, began to
recognize that they were a marked group. It became increasingly
apparent that these men had more exposure than was officially
acknowledged and that they were sicker than they should be. Their
sicknesses didn't fit any category that the Veterans
Administration was going to recognize as convincible as service
connected. Then it became increasingly apparent that these men
didn't really have the kind of disorders, at least some of them,
that other people had. Again, here is where time makes a lot of
difference. Had I been a young physician, I wouldn't have been
secure about being able to tell the difference between malingering
or psychoneurotic or opportunistic complaints. After 40 years in
a mill town, you really do begin to know how to tell what is real
disease, what is imagined disease and what is feigned disease. It
was very clear as you reviewed, and I reviewed close to a couple
of hundred by now, medical records, that many of these men had an
exposure to ionizing radiation of sufficient and significant
degree so that they were sure that they had been exposed but not
enough for them to have had a recognized and officially
acknowledged diagnosis of acute radiation sickness. Many times
they would go to see the doctor at the VA or on duty in the
military service or subsequently in civilian life and the doctor
would say, "You had radiation sickness." But then when push came
to shove, it turned out that the records said that the guy had had
too much sunburn and too much beer, and that is why he got skin
rash, nausea and vomiting, and bloody diarrhea. So the official
records more often than not never had it.
Over and over again you would find that the guy who knew all
his buddies and had pictures of where he had been at the Nevada
test sites would write in and there would be no record of his ever
having been there until he pushed and pushed and finally got his
lawyer to write a freedom-of-information act letter. Then they'd
say, "Oh yes, he was there." After awhile they'd say, "Our
records got burned up in St. Louis," or "Our records got lost,
mislaid or incomplete, so we will accept any veteran's assertion
that he was there on face value if we don't find the records to
the contrary." Then it became apparent that these guys were sick
and they couldn't really identify what their major difficulty was
except that they had never felt quite up to what they should be.
There were lots of malingerers, constitutionally inadequate people
who were never able to face life. This was different. These guys
had specific complaints, and later you could find objective
physical findings that didn't fit other categories of disease.
This has become so apparent in so many of the records. I think
that probably 10% of the hundreds of cases that I have reviewed
closely, and have reviewed in general with other people who are
concerned with this problem, had this syndrome. It is almost
surely got to do with the nature of ionized radiation which does
not hit this organ or that organ or this part of the body or that
part of the body, but will go through the body and hit at random
any molecule in any chemical constituent or any part of the cell.
The cell is a great big thing, as big as the human being when you
can start thinking in terms of molecules. There are billions of
molecules in just the chromosome. The chromosome is only a small
part of the nucleus, and the nucleus is only a small part of the
cell, and the cell is made up of all sorts of complex things, each
of which is made up of molecules, which have got hundreds of
thousands of atoms in them, and each of the atoms has a number of
circulating electrons. Ionizing radiation pings off these
electrons in these atoms, in these molecules, in these fragments
of cell, and the guy just doesn't feel right. It may kill the
cell and then it gets replaced with fibrous tissue or it may
change the protein that makes other proteins, that makes other
enzymes, and they are all a little bit off, so you couldn't know what was going to happen. If you'd look, you would find that this
does actually happen at very, very, very low levels of ionizing
radiation. Most of the x-rays that we have taken, chest x-rays,
diagnostic x-rays, are measured in thousands of electron volts;
and if you take a series of them, you just multiply them. You can
disrupt things with very small amounts. Then it gets more and more
complicated, but this has been the problem as I have seen it. I
came at it, being a clinician, from a clinical aspect.
I came at it from hearing men tell their stories about what
has happened to them. To put their stories together in a
cause-and-effect relationship to something that happened to them
35 years ago is impossible, and that is what has been known as the
doctors dilemma. But if you see these stories and you see these
patterns of disorder happening over and over again, and you
recognize the molecular and physical and chemical basis, that that
is the way radiation works, then it not only justifies it but it
explains why it is the way it is. That is where we are at the
present time. This has all been complicated by the fact that
since the day after Hiroshima, everything to do with the human
hazards of ionizing radiation has been relegated to the Department
of Energy. It was originally the Atomic Energy Commission in the
military, but now under the Department of Energy, and 27 national
radiation laboratories and what is known as the Oak Ridge
Associated Universities, Oak Ridge, Tennessee, one of the major
radiation facilities government run. The 80 Oak Ridge Associated
Universities are the key universities throughout the country that
have big nuclear physics facilities, and they are all very well
dominated by men who understand what shall and what shall not be
disseminated for general consumption. You go to the government
documents catalogue and everything you get out of there is
stamped, "Cleared, Unlimited Distribution," which means that there
are other things that are not cleared. So that I have persuaded,
having spent a lot of time studying how radiation works
particularly in human tissues, I have persuaded there are a number
of very good scientists and health physicists and physicians who
are equally assured that this is indeed a fact and that we have
absolutely no idea of the degree to which damage is being done. I am not saying it is absolutely destructive. I am just saying the
evidence is that it is far more destructive than the general
public has been allowed to believe. So that is what I am doing
right now.
Almost 20 years ago the high school kids saw their
out-of-high school colleagues meet right here across the street on
the common in front of the town hall. One night one of the young
people that I knew very well shouted, "Dr. Boardman," right from
the monument out here, and called because one of his buddies was
over there with an overdose, I guess it must have been heroin
because he had a respiratory arrest. They got the EMT, and the
EMT gave him artificial resuscitation and took him off to the
hospital; but it was as blatant as that -- the teenagers
collecting night after night out here in front of the town and
exchanging and smoking a lot of pot, etc. Two of the younger
doctors of the Acton Medical Associates, Jim Longcope, who is now
a psychiatrist on staff of Emerson, and Bob Shumacher, who is a
pediatrician who went out to the Indian service for awhile and
then came back to a private pediatric practice in New Hampshire,
got together with some of these young people, who we knew as
patients and as contemporaries of some of my children, and we had
about 25 enlisted people who came every Tuesday evening to talk
about the drug problem. I've always thought it would be a good
idea for us to do a follow-up. Well, with 25 that we knew of, the
general agreement was that there were at least 50 mainline
shooters, intravenous heroin users, in our community. That
included Concord, and I don't know how far beyond Concord, Acton
and Maynard. We figured at that time that 50 hard-drug users in a
community of a few thousand represented a higher incidence of
heroin addicts in our community than was reported in New York
City. That made us sit up and take notice, and so we started
talking about it, and talked to these guys, and talked about how
useless it was and what a dead-end track it was on. We never
felt, the three doctors, that we really had much impact other than
we represented the established community who was willing to talk,
listen, and appreciate them as individual human beings. Who's to
say whether that had any effect? All I can say is at least one of them got on the methadone and became a lawyer, another one has
been in and out of rehabilitation for the next ten or twenty
years, one turns up every now and then and reports to me on some
of the others, and to my knowledge none of them are dead yet. Of
course, here it is '89 -- it is almost another 10 years, it is
almost 20 years. One of them really kicked the habit entirely and
became a laboratory supervisor in one of the teaching hospitals in
Boston, and his sister also was able to kick the habit. So some
of them got off it, some of them are still struggling with it,
some of them are lost to it. When I came back from Africa, it was
ten years from this Tuesday evening group, I asked around if the
drugs were any less. Those who were in the know said, "On the
contrary, it is probably much worse, it is much more undercover,
and it is a much younger group." I never undertook to get
involved with it again. Perhaps I should. I thought perhaps
somebody else should becoming involved again.
I guess I would say the older I get, the later it gets into
the century, the longer I watch the common scene, the more
impressed I am with the general lack of interpersonal
communication and interhuman compassionate awareness we have for
one another, not only in medicine, not only in nuclear energy, not
only in the high-tech modern medical management, but in every
aspect of human endeavor. I think we are in very precarious
times. I don't believe that I am alone. Bill Moyer has been
having people provide a world of ideas near midnight for the last
month. Everything that those people said sounded very familiar to
me and really very ominous. Of course, we all end up on a note of
hope. It has got to be better. It is too good to be over with.
It seems to me that Albert Einstein was speaking far more
profoundly than people have ever understood when he said, "We have
got to change our way of thinking." We have got to change our way
of thinking, our way of feeling, our way of interrelating, our way
of caring not only for one another but for the earth itself and
for everything that it stands for. We are making absolutely
obscene clutter of the cosmic surroundings of the earth, filling
it with radioactive satellites, so it is beginning to look like a
used car lot, and we do it with an absolutely pre-adolescent arrogance of ignorance, of not having any sense of responsibility
of what we are doing in a very real way to potentially upsetting
the total cosmic relationship of this single isolated globe. I
feel that this is truly disastrous, and I honestly believe I want
to live to see whether humanity can change its way by the turn of
the century. I think the year 2000 between here and there is
very, very precarious. If we make it to the year 2000, we will
have made such compromises with our arrogance that we will bumble
along for another 3000 years. I think between here and there is
very, very questionable.
I spent a lot of time in the cardiac outpatient department at
Boston University School of Medicine, as well as working in the
medical clinic, and I was much interested in taking care of
cardiac patients along with Jim Hitchcock at Emerson Hospital. I
had been doing electrocardiography ever since I was studying at
Mass. General as a medical student. Emerson Hospital was ready
for a coronary care unit. With Pat Snow and some of the nurses in
the east wing, we designed cutting windows and mirrors to make an
intensive care unit where the nurses could sit and see each of six
beds from where she sat. Then we got American Optical
oscilloscope for cardiac monitoring for these patients, and we
were in business. Charlie Keevil wrote it all up, and it was one
of the key features of Emerson Hospital's contribution to
community health care.